Prefinal Practical examination
This is an online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
This E blog also reflects my patient centered online learning portfolio and your valuable inputs on the comment box is welcome.
I have been given this case to solve in an attempt to understand the topic of " patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings investigations and come up with diagnosis and treatment plan.
A 67 year old male resident of miryalaguda occupation by barber came to medicine opd with
Chief complaints :
Fever since 4days
burning micturition since 4days
decreased urine output since 3days
Abdominal pain in the left side:-2days
HOPI :
Patient was apparently asymptomatic 4 days ago and then developed fever which was insidious in onset,intermittent,associated with chills and rigors,burning during micturition and decreased urine output.
From 2days patient is having pain in the left side of abdomen—insidious onset,intermittent,Migrating from loin to groin,colicky type of pain.
Fever is not associated with cough, vomiting, loose stools,pedal edema
PAST HISTORY:
Urinary complaints of frequency and urgency since 1 yr along with burning micturition.
3months back patient developed fever went to local hospital got medicines ,even after taking medication symptoms are not relieved
K/c/o hypertension since 10 yrs,using medication
Bilateral knee pain since 5 yr bcz of which he stopped farming.
PERSONAL HISTORY:
Patient wakes up at 6: 30 am and he drinks tea and take breakfast ( chapati , dosa , idly ) .At 8:30am he walks for 1km to reach his saloon shop work till 1:00pm and walks back for lunch to home. He has his lunch ( rice , any curry and curd ) takes a rest till 4 pm . In evening routine he eat snacks of tea and biscuits and watch telivision till 9pm , occasionally drinks alcohol and in dinner he eat rice with dal and vegetable curry and sleeps by 10:00pm
Diet:mixed
Sleep:regular
Bladder - burning micturition +
Bowel movements are regular
Addictions:he started taking chewable tobacco since 30 years
alcohol since 25 years
Family history:
Young brother died with HIV
no similar complaint
GENERAL EXAMINATION:
Patient is conscious,coherent , cooperative with time, place, person
Vitals:
BP-120/80mmhg
PR-84 bpm,regular rhythm, normal volume
RR- 24cpm
Jvp - not elevated
Grbs- 120 mg/dl
Poor oral hygiene (Tobacco staining on upper inner teeth)
Pallor - present
No icterus,
No lymphadenopathy,
No cyanosis,
No clubbing,
No edema.
SYSTEMIC EXAMINATION:
RESPIRATORY SYSTEM:
Patient examined in sitting position
Inspection:-
Upper respiratory tract- external nose normal,oral cavity- poor oral hygiene,no halitosis,no thrush
Chest appears bilaterally symmetrical & barrel shaped.
Respiratory movements appear equal on both sides and its Abdominothoracic type.
Lower respiratory tract- trachea appears central,no scars,dilated veins over chest,apical impulse not visible,chest bilaterally symmetrical and movements equal on both sides
Spinal deformity- kyphosis
Palpation:-
All inspiratory findings confirmed
Trachea central in position
Apical impulse in left 5th ICS, 1cm medial to mid clavicular line
Tactile Vocal fremitus
infraclavicular-normal
Mammary- normal
Axillary-normal
Infra mammary-normal
Suprascapular-normal
scapular- normal
Infrascapular-normal
AP diameter- 26cms,transverse diameter- 26cms
Percussion: resonant-normal.
Auscultation:normal vesicular breath sounds with no added sounds
Vocal resonance normal.
PER ABDOMEN:
Inspection:-
Shape of abdomen-scaphoid
Normal contour
Umbilicus is inverted
No scar,pigmentation, engorged veins ,peristaltic waves
All quadrants are moving equally with respiration
Hernias orifices normal
Palpation:-
NO local rise of temperature and Tenderness
No Palpable mass
Liver- Not palpable
Spleen - Not palpable
Bimanual examination-kidney is not palpable on left and right side
Percussion:-
tympanic resonance is heard
Auscultation:-
Bowel sounds are heard
CVS:
Inspection :
Shape of chest- barrel
No engorged veins, scars, visible pulsations
Palpation :
Apex beat can be palpable in 5th inter costal space
Auscultation :
S1,S2 are heard
no murmurs
CNS: No focal neurological deficits found
Level of Consciousness- Conscious
Speech - Normal
Signs of Meningeal Irritation
Neck Stiffness - No
Kerning's Sign - No
Cranial Nerve-normal
Motor System- Normal
Sensory System- normal
Glasgow Scale- normal
Finger - Nose In - Coordination - No
Knee - Heel In-coordination - No
Provisional Diagnosis: Lower urinary tract infection
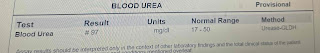
Investigations:
Final diagnosis:
Urinary tract infection
Post renal aki secondary to left ureteric obstruction -?mass/strictures
K/c/o htn since 10 years
Normocytic normochromic anemia
Kyphosis


















Comments
Post a Comment